A) Location
B) Device
C) Body System
D) Approach
Correct Answer

verified
Correct Answer
verified
Multiple Choice
What is the lowest level of medical complexity represented by CPT E/M codes?
A) straightforward
B) problem-focused
C) low complexity
D) detailed
Correct Answer

verified
Correct Answer
verified
Multiple Choice
Which code set is alphanumeric?
A) ICD-10-PCS
B) NDC
C) CPT-4, Category 1
D) SNOMED CT
Correct Answer

verified
Correct Answer
verified
Multiple Choice
Why is electronic data interchange (EDI) beneficial?
A) computers can exchange information without human intervention
B) information can only be "read" by the recipient
C) messages contain unique identifiers that cannot be duplicated
D) it works across reimbursement and clinical platforms
Correct Answer

verified
Correct Answer
verified
Multiple Choice
Tracking codes to determine the volume of cases seen at the facility is a _____________ use of coded data.
A) outcomes measurement
B) research
C) reimbursement
D) resource utilization
Correct Answer

verified
Correct Answer
verified
Multiple Choice
Which statement about SNOMED CT is false?
A) it can assign codes from free text
B) it makes systems interoperable across countries and languages
C) there is a one-to-one translation between SNOMED CT and ICD-10-CM
D) it has the potential to be useful during patient care, rather than after
Correct Answer

verified
Correct Answer
verified
Multiple Choice
In which case would a CDI physician champion be involved?
A) a provider and a clinical documentation improvement specialist disagree on what should be included in the plan of care
B) a nurse is slow to input progress notes
C) a coder adds complications and comorbidities that are unsupported by documentation
D) a provider will not authenticate his verbal orders in a timely manner
Correct Answer

verified
Correct Answer
verified
Multiple Choice
The Health Insurance Portability and Accountability Act (HIPAA) of 1996 required the:
A) reporting of diagnosis data to the National Center for Health Statistics (NCHS) .
B) adoption and use of ICD-10-CM.
C) use of the EHR with point-of-care data capture.
D) use of certain codes in electronic transmissions.
Correct Answer

verified
Correct Answer
verified
Multiple Choice
The _________ axis of an ICD-O-3 code indicates the site of a neoplasm in the body.
A) morphology
B) oncology
C) topography
D) pathology
Correct Answer

verified
C
Correct Answer
verified
Multiple Choice
____________ occurs when the coding results in the MS-DRG that most accurately represents the facility's utilization of resources, on the basis of the diagnoses and procedures, and is completely substantiated by documentation.
A) Maximization
B) Validity
C) Optimization
D) Compliance
Correct Answer

verified
C
Correct Answer
verified
Multiple Choice
An example of a CPT-4 (Health Care Common Procedure Coding System [HCPCS] Level 1) code is:
A) C1715
B) 0DJD8ZZ
C) 4557003
D) 43251
Correct Answer

verified
Correct Answer
verified
Multiple Choice
The auditor was reviewing the hospital bills and noticed that for several cases billed to a commercial payer the DRG assignment, based on the MS-DRG description of the DRG code, did not match the diagnosis/procedure codes. One possible reason for this is:
A) the coder made an error assigning the DRG.
B) the grouper isn't working properly.
C) that payer uses a different DRG than Medicare.
D) the MS-DRG description is incorrect.
Correct Answer

verified
C
Correct Answer
verified
Multiple Choice
Which organization is NOT one of the four Cooperating Parties for the ICD-10-CM?
A) American Medical Association (AMA)
B) Centers for Medicare and Medicaid Services (CMS)
C) National Center for Health Statistics (NCHS)
D) The Joint Commission (TJC)
Correct Answer

verified
Correct Answer
verified
Multiple Choice
It is the coder's responsibility to assign codes completely and accurately so that a facility receives the reimbursement to which it is entitled. To meet this responsibility, a coder must:
A) follow all software prompts that will add a "cc" code. The software program is written so that the coder does not have to review the medical record.
B) use coding software to sequence the best principal diagnosis for the highest reimbursement.
C) code and sequence according to the documentation in the medical record, using the software to optimize the coding.
D) adjust the principle diagnosis as needed to achieve the right DRG for the patient's needs.
Correct Answer

verified
Correct Answer
verified
Multiple Choice
Why are coding audits performed by payers insufficient for determining coding accuracy?
A) the payer only checks records for the patients they have reimbursed
B) the payer only performs targeted reviews on "problem" DRGs
C) payers will only audit when there is a change in case mix
D) payers are ultimately more interested in volume rather than accuracy
Correct Answer

verified
Correct Answer
verified
Multiple Choice
Why might a coding manager automatically review and/or revise patients assigned to DRG 469 (MAJOR JOINT REPLACEMENT OR REATTACHMENT OF LOWER EXTREMITY W MCC) or DRG 470 (MAJOR JOINT REPLACEMENT OR REATTACHMENT OF LOWER EXTREMITY W/O MCC) ?
A) The hospital might not be entitled to the reimbursement for these DRGs.
B) The federal government always reviews these DRGs for fraud and abuse.
C) There is something incorrect with the codes assigned and/or data when a patient is grouped into either of these DRGs.
D) These DRGs are on the OIG workplan this year.
Correct Answer

verified
Correct Answer
verified
Multiple Choice
Which is an appropriate measure of the success of a clinical documentation improvement (CDI) program?
A) a more complex case mix
B) higher reimbursements
C) shorter average length of stay
D) diagnosis documentation changes
Correct Answer

verified
Correct Answer
verified
Multiple Choice
The NDC code for one 28-tablet bottle of the chronic hepatitis medication Harvoni, made by Gilead Sciences, is 61958-1801-1. The number "61958" is the
A) labeler code
B) product code
C) packaging code
D) batch code
Correct Answer

verified
Correct Answer
verified
Multiple Choice
Using the figure, which is the ICD-10-PCS code for an endoscopic colonoscopy? 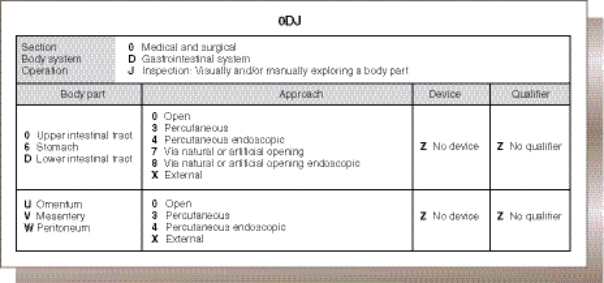
A) ODJD8ZZ
B) ODJD7ZZ
C) ODJ68ZZ
D) ODJ67ZZ
Correct Answer

verified
Correct Answer
verified
Short Answer
Level _____________ of HCPCS is also known as Current Procedural Terminology (CPT).
Correct Answer

verified
Correct Answer
verified
Showing 1 - 20 of 54
Related Exams